
Dirección Xeral de Saúde Pública Galicia
Cannabis
Abstract: Abstract
Cannabis is the most widely used illegal psychoactive substance among young individuals. Early onset of use is associated with problems in school performance and early school drop-out, as well as an increased presence of mental disorders (anxiety, depression, psychosis) in adulthood. Earlier use and higher frequency of use indicate greater risks.
Keywords: cannabis; epidemiology; intervention
INTRODUCTION
In recent years, greater attention has been paid to the potential
public health implications of cannabis use. This is due to several
reasons, among them, the widespread use of cannabis among the
Spanish and European population in general, the increased number of
demands for dependency treatment, and the increased number of
conditions associated with cannabis use.
Cannabis is a plant containing over 421 chemical compounds, 61 of
which are cannabinoids, with D9-THC having the highest psychoactive
capacity and contributing the most to the toxicity of cannabis.
The onset of cannabis use typically begins before the age of 15
and is more frequent in males, who have a higher prevalence of use
of other related drugs (alcohol and tobacco).
The onset of cannabis use has to do with many factors, one key
factor being “peer pressure”, compounded by the low risk perceived
by the youngest, which leads to the normalisation of cannabis use in
these age groups.
Easy access to this drug (even if it is an illegal psychoactive
substance) means that there is now a higher incidence of consumption
among the younger population.
DATOS EPIDEMIÓLOGOS
Cannabis remains the most widely used illegal psychoactive
substance in Europe, in all age groups
(Informe Europeo sobre Drogas Tendencias y novedades, 2018)
.
This psychoactive substance is usually smoked and, in Europe, is
often mixed with tobacco. Cannabis use patterns range from
occasional to regular to dependent use. Most cannabis users are
experimental or occasional users. However, in a significant
proportion of cases, the pattern of cannabis use increases the risk
of suffering health effects, poor academic and work performance,
and/or developing a dependency.
About 26.3% of European adults (15-64 years) are estimated to
have used cannabis at some point in their lives. Of these, it is
estimated that 14.1% of young adults (15-34 years old) used cannabis
in the last year, 17.4% of them between 15 and 24 years old. Among
those who consumed this psychoactive substance during the last year,
the ratio of males to females was two to one.
The results of the latest survey show that, in most countries,
cannabis use has either remained stable or increased among young
adults over the previous year.
According to the Survey on the Use of Drugs in Secondary
Education in Spain
(Ministerio de Sanidad Consumo y Bienestar Social, 2016)
, the consumption of cannabis was
slightly more widespread among males: 15.2% of 14-year-olds had used
cannabis at some point (as compared to 12.6% of females), a
proportion that increases progressively with age, to the point that,
one in every two 18-year-old males (56.3%) had already used it at
some point (as compared to 54.7% of females). Cannabis users also
report a higher prevalence of alcohol and tobacco use.
IMPACT ON THE BODY
Cannabis may be used in the following ways: through inhalation
(mixed with tobacco, vaporised, using a pipe or an electronic
cigarette) or orally (in cookies/cakes, etc.).
Its effects on the body are produced by the activation of
specific cannabinoid receptors (the CB1 receptor, which is
abundantly located in the CNS, and the CB2 receptor, which is
expressed primarily on the cells of the immune system). The
activation of these receptors produces the inhibition of the release
of neurotransmitters from axon terminals.
Cannabis use generally produces depressant-type effects, mild
euphoria, and alterations in perception (distortions in time
perception, intensified regular sensory experiences). It may also
produce anxiety, panic, paranoia, psychosis, depression, inhibition
of motor skills, as well as muscle relaxation.
These reactions are dose-dependent.
Immediately after consumption “cannabis intoxication” occurs,
with symptoms like dry mouth, red eyes, tachycardia, lack of
movement coordination, uncontrolled laughter, drowsiness, and
alterations in memory, attention, and concentration.
ADRESSING CANNABIS USE
It is important to make an early detection of cannabis use in
order to intervene as soon as possible on the individual and their
environment by offering personalised care. Paediatric professionals
should inform parents when they detect any “warning signs”.
Suspicion of consumption. Warning signs:
-
Behaviour and mood shifts.
-
Neglect of personal hygiene.
-
Deterioration of family relationships and their environment
in young individuals.
-
Poor academic performance.
-
School absenteeism.
If cannabis use is detected, a brief intervention should be
conducted. If such use becomes problematic, the minor may require an
intensive intervention, in which case referral to a specialised unit
might be considered.
Myths about cannabis
As in the case of tobacco, there are misconceptions that have
become entrenched in society regarding cannabis consumption which
must be clarified by professionals.
Many of the misconceptions or myths about cannabis going around
are related to it being innocuous, posing a low health risk because
it is a “natural product”, or being therapeutically useful.
This confusion generated around cannabis consumption, which is
directed at the most vulnerable population, requires interventions
on the part of health professionals, who must provide the general
population with correct information. Only in this way may these
myths be debunked.
DIAGNOSTIC TOOLS
There are useful tools for detecting patients at risk of cannabis
use from the primary healthcare perspective.
There are several scales for assessing cannabis use. The CAST
scale
(Cuenca-Royo et al., 2012)
is a simple 6-question
questionnaire, developed in France, with the aim of detecting
problematic consumption patterns. Ever since this scale was
developed, it has been widely used both in the general population
and in the adolescent population in several countries, and has
proven to be suitable for this purpose.
The use of this scale in primary care would facilitate the
identification of young individuals who may be at risk of developing
a cannabis use disorder, guide the diagnosis, and help them be
referred to specific treatment programmes.
Table 1. CAST. Cannabis Abuse Screening Test
Table 1. CAST. Cannabis Abuse Screening Test
| CAST. Cannabis Abuse Screening Test |
-
Have you smoked cannabis before midday?
-
Have you smoked cannabis when you were alone?
-
Have you had memory problems when you smoked
cannabis?
-
Have friends or family members told you that you should
reduce or stop your cannabis consumption?
-
Have you tried to reduce or stop your cannabis use
without succeeding?
-
Have you had problems because of your cannabis use
(argument, fight, accident, poor results at school,
etc.)?
|
Results:
See Figure Figure 1 Esquema de Intervención según el CAST
Figura 1 Esquema de Intervención según el CAST
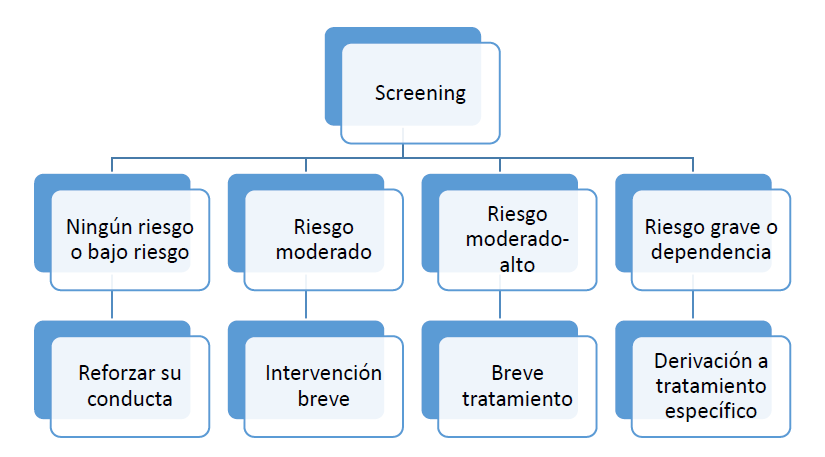
Fuente: (Legleye, Karila, Beck, & Reynaud, 2007)
Translation Table 2. Spanish – English Figure 1. Intervention plan according
to the CAST scale
Table 2. Spanish – English Figure 1. Intervention plan according
to the CAST scale
|
Spanish
|
English
|
|
Screening
|
Screening |
|
Ningún riesgo o bajo riesgo
|
Little to no risk |
|
Riesgo moderado
|
Moderate risk |
|
Riesgo moderado-alto
|
Moderate-to-high risk |
|
Riesgo grave o dependencia
|
High risk or dependency |
|
Reforzar su conducta
|
Behaviour should be reinforced |
|
Intervención breve
|
Brief intervention |
|
Breve tratamiento
|
Brief treatment |
|
Derivación a tratamiento específico
|
Specific treatment referral |
Interventions in minors will be different depending on the
following:
-
If parents are aware of the minor’s cannabis consumption, the
minor will be asked for permission to include their parents
during the interventions.
-
If parents are not aware of the minor’s cannabis consumption,
the age of the patient and the degree of risk identified after
the screening will be taken into account before including
parents in the interventions.
Different actions should be taken based on the results
-
If no risks are identified, beneficial aspects should be
emphasised and positive and healthy choices should be
reinforced.
-
In the case of non-problematic users, brief pieces of
advice should be provided:
-
I’d recommend you against doing it again. Your brain is
still developing, and using cannabis or other psychoactive
substances may affect its proper development.
-
Cannabis use may interfere with your decision-making and
may cause you to act inappropriately.
-
In the case of problematic consumers, more intensive
interventions are needed. Establish an action plan with the
user, including individualised and personalised
objectives:
-
Agree to a withdrawal for a certain period of time (4-8
weeks), with the goal of making them aware of the
seriousness of their problem.
-
Establish strategies to avoid consumption.
-
Monitoring and reinforcing the milestones achieved.
If these objectives are not achieved, refer to a specialised
unit.
GENERAL RECOMMENDATIONS FOR PAEDIATRIC
PRACTICE
Paediatric professionals should emphasise the following
points:
-
Cannabis is addictive.
-
Cannabis use is closely related to the consumption of other
substances (alcohol and/or tobacco).
-
THC (tetrahydrocannabinol) is the main active ingredient in
cannabis. It is a very fat-soluble substance that reaches the
brain quickly, where it accumulates, and the body eliminates it
eliminated very slowly. It has long-term effects: cannabis
consumption during weekends tend to accumulate, since one week
after consumption, the body has still not managed to eliminate
more than 50% of the substance.
Even if an individual only consumes cannabis at the weekends, it
is not enough time for the body to eliminate it completely and it
will therefore accumulate in the brain, producing different
effects.
-
Cannabis use is associated with poorer or failed academic
performance. The negative effects of cannabis use on attention,
motivation, memory, and learning skills may last for days and
even weeks after the immediate effects have worn off.
-
Like most psychoactive substances, cannabis use may impair
decision-making skills, which may be conducive to engaging in
risky behaviours.
-
Attention should be paid to the occurrence of symptoms of
accidental cannabis poisoning in previously healthy children who
now present with acute neurological symptoms for unknown
reasons. It may be useful to make a differential diagnosis with
other conditions such as hypoglycaemia, CNS infections, etc.
Urine toxicology testing should be requested to confirm acute
exposure to cannabis.
-
Smoking cannabis during lactation is a risk factor for sudden
infant death and has been associated with delayed motor
development at one year of age. The fat-soluble nature of
cannabis causes THC to accumulate in breast milk up to 8 times
more than it does in the mother’s body.

 License Creative Commons Attribution -NonCommercial-ShareAlike 4.0 International
License Creative Commons Attribution -NonCommercial-ShareAlike 4.0 International