
Sara Martín Armentia and Alicia Armentia Medina
Recommendations for Preventing, Diagnosing and Treating Food Allergy in Children
Abstract: AbstractThere is a wide range of adverse food
reactions. Allergic reactions must be distinguished from toxic
reactions and non-toxic reactions, which are not-immune mediated. Food
allergies may be divided into two groups: IgE-mediated food allergies,
in which immediate clinical features appear on contact with the
allergen, and non-IgE-mediated food allergies, which have a prolonged
latent period and a more insidious onset.Most cases of food allergy develop in the first two years of age,
with a peak of 8% in one-year-olds. The main causative foods in
children are milk, eggs, and fish.The basis for diagnosing an allergy is the clinical record, in
which suspicious allergy symptoms must be registered: hives, asthma,
atopic dermatitis, anaphylaxis, etc., as well as in vivo complementary
tests (prick tests, provocation tests, elimination diet) and in vitro
complementary tests: specific IgE determination and molecular
diagnostics. The therapeutic options are based on a diet of
elimination of the causative food. After the diagnosis, patients
should be monitored until the natural acquisition of tolerance to food
is verified and, should this not be achieved, hyposensitisation
treatment, such as allergen-specific oral immunotherapy, should be
initiated.It must be borne in mind that patients with food allergy may become
sensitive to other foods. In children allergic to milk, a plan must be
established for the progressive introduction of solid foods, and the
appearance of allergy symptoms must be monitored.The optimal follow-up of a child with food allergy requires the
collaboration of the paediatrician and the allergist, and in order to
find the correct aetiology, valid diagnostic techniques must be
used.
Keywords: Allergy; food; children; IgE; prick test; immunotherapy; tolerance
INTRODUCTION
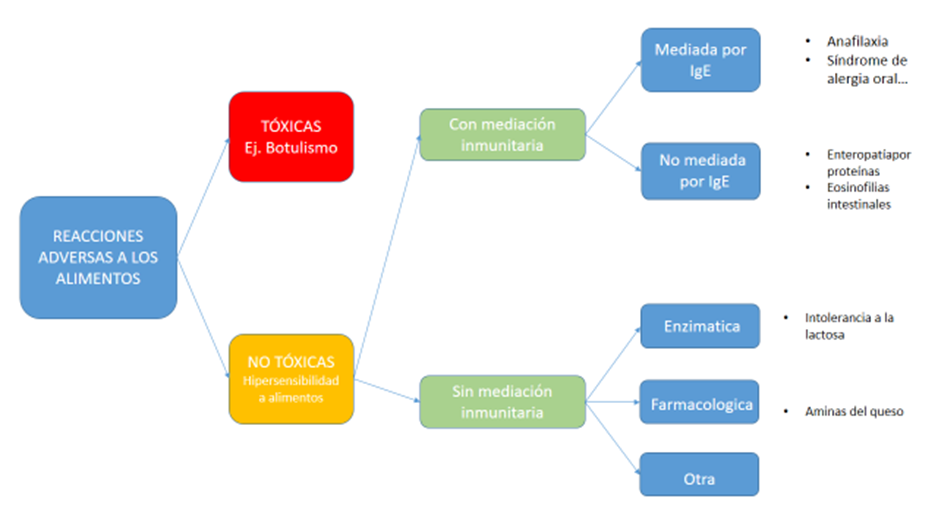
Recently, the Nomenclature Committee of the European Academy of
Allergy and Clinical Immunology
(Worm, 2014)
proposes that any
adverse reaction to food be defined as food hypersensitivity.
Allergic reactions should be distinguished from toxic food reactions
(botulism, toxic oil syndrome, etc.) and from non-toxic,
non-immune-mediated reactions (previously known as food
intolerance), such as lactose intolerance, or metabolic conditions,
such as phenylketonuria (
Figure 1. Classification of the main adverse food reactions.)
(Translation Figure 1. Classification of the main adverse food reactions)
A particular characteristic of
the latter two is that they depend on the dose ingested, i.e. the
intensity of clinical features depends on the amount of food the
individual has been exposed to. Other examples in this
group are drug hypersensitivity reactions to natural adjuvants or
compounds added during food processing.
Figure 1. Classification of the main adverse food reactions
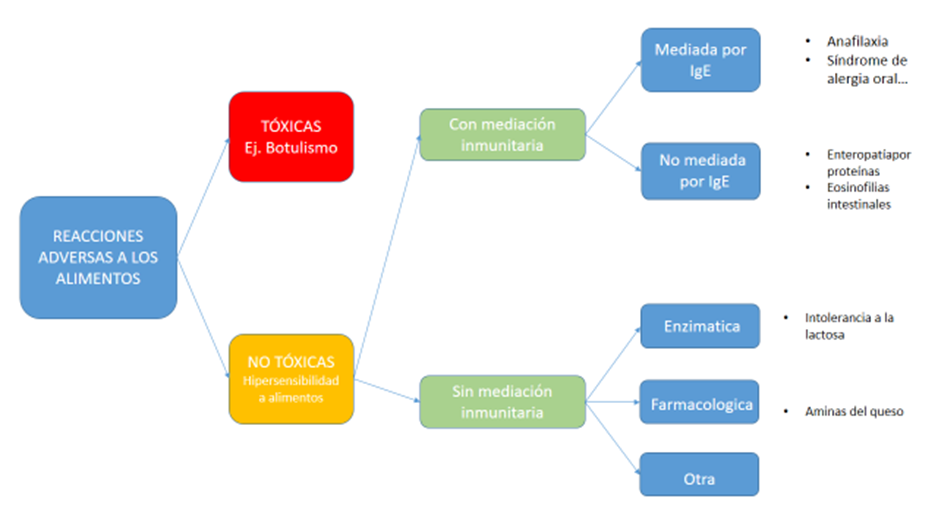
Source: Compiled by the authors
Table 1. Translation Figure 1. Classification of the main adverse food reactions
|
Spanish
|
English
|
|
REACCIONES ADVERSAS A LOS ALIMENTOS
|
ADVERSE FOOD REACTIONS
|
|
TÓXICAS
Ej. Botulismo
|
TOXIC
e.g. botulism
|
|
NO TÓXICAS
Hipersensibilidad a los alimentos
|
NÃO TÓXICAS
Food hypersensitivity
|
|
Con mediación inmunitaria
|
Immune-mediated
|
|
Sin mediación inmunitaria
|
Non-immune mediated
|
|
Mediada por lgE
|
IgE-mediated
|
|
No mediada por lgE
|
Non-IgE-mediated
|
|
Enzimática
|
Enzymatic
|
|
Farmacológica
|
Drug-related
|
|
Otra
|
Other
|
|
- Anafilaxia
- Síndrome de alergia oral…
|
- Anaphylaxis
- Oral allergy syndrome…
|
|
- Enteropatía por proteínas
- Eosinofilias intestinales
|
- Protein enteropathy
- Intestinal eosinophilia
|
|
- Intolerancia a la lactosa
|
- Lactose intolerance
|
|
- Aminas del queso
|
- Amines in cheese
|
However, in immune-mediated hypersensitivity reactions
(food allergy), very small doses of food may result in exaggerated
clinical features. Food allergies may be divided into two groups,
depending on whether or not the symptoms are IgE-mediated.
IgE mediated food allergies often produce immediate clinical
features on contact (by ingestion or inhalation) with the allergen:
hives, angioedema, asthma. Non-IgE-mediated food allergies
have a prolonged latent period and a more insidious onset,
mainly affecting the digestive tract
(Martín Mateos, 2011).
STRUCTURED QUESTION
What would be the most appropriate management of a suspected food
allergy in children?
EPIDEMIOLOGY OF FOOD ALLERGY
Up to one-third of all families have visited the
paediatrician at some time on suspicion of an adverse reaction to
food
(Pyrhönen, Näyhä, Kaila, Hiltunen, & Läärä, 2009)
(Leung, Yung, Wong, Lam, & Wong, 2009)
(Venter et al., 2006).
An estimated 10% of these visits may be due to an immune
reaction. Data on food allergy prevalence are limited due to the
disparity of criteria, survey methodologies, and populations. Most
food allergies appear in the first two years of life, with a peak of
8% in one-year-olds, as it is during the first years of life that
most potentially allergenic foods are introduced into the diet and
when immune tolerance mechanisms are established. This prevalence
decreases as the child grows older, remaining at 3-4% in
adulthood
(Nwaru et al., 2014).
Etiology
According to data from the Spanish multicentre study
Alergológica
(SEAIC, 2015)
,he main food allergens
in children are milk (82%), eggs (76%), and fish (50%). In adults,
nuts (35%), fresh fruit (31%), fish, shellfish, and eggs (10%).
However, these percentages differ according to specific
geographical areas and dietary habits.
Diagnosis
The clinical record and complementary tests are the basis
for the diagnosis of food allergies
Clinical features in relation to food allergy:
-
Hives and/or angioedema are the most
frequent signs. Hives (urticaria) usually appear suddenly,
together with intense itching, mainly affecting the skin that
has been in contact with the food (face, mouth, and hands).
Oedema and swelling of soft tissues (angioedema) may also
occur, with glottic oedema being the most dangerous, as it
compromises the respiratory tract.
-
Acute gastrointestinal symptoms:
nausea, vomiting, abdominal pain, or sudden-onset diarrhoea
after eating the food. Generally in infants, rare in older
children. Special mention should be made of the
Food Protein-Induced Enterocolitis Syndrome (FPIES) or
food-induced enterocolitis, which is a non-IgE mediated
allergy.
-
Oral allergy syndrome: Oral or
oropharyngeal pruritus after eating certain foods, usually
fresh fruits and vegetables. This syndrome occurs very
frequently in patients with allergies to pollen (grasses) and
sometimes precedes a more serious condition: anaphylaxis. It
can be prevented if vegetables are cooked.
-
Atopic dermatitis: Dryness,
erythema, and skin irritation. In atopic dermatitis, it is
common to find lgE-mediated hypersensitivity to various foods
and inhalants, although the severity of dermatitis is not
associated with food. It is necessary to establish the true
clinical meaning of these lesions via elimination diet and the
subsequent controlled provocation.
-
Bronchial asthma: Dyspnoea during
bronchoconstriction and hissing respiration during
auscultation. In highly food-allergic patients, asthma or
pharyngo-conjunctival symptoms (conjunctivitis, rhinitis) may
occur after inhalation of volatile food products that are more
intensely released during handling or cooking.
-
Anaphylaxis: Up to 1% of patients
sensitised to food may present with anaphylaxis. This is a
very serious allergic reaction: it should be suspected when
there is skin impairment immediately after the ingestion of a
food (hives, angioedema). Associated clinical features in
other systems: respiratory system (asthma, uvular oedema),
digestive system (diarrhoea, vomiting). Sometimes several
systems can be affected and lead to shock, so it is necessary
to be familiar with anaphylaxis to treat it before it
escalates to shock.
Apart from these clinical features, there are multiple
food allergy-related conditions, generally non-IgE-mediated
Table 1. Examples of non-IGE-mediated food allergies.
Table 2. Examples of non-IGE-mediated food allergies IgE
|
Enfermedad celíaca
Dermatitis herpetiforme
Enteropatias por alimentos
Eosinofilias intestinales (gastritis, esofagitis
eosinofílica)
Proctocolitis alérgica
|
Neumopatía por hipersensibilidad a la leche de
vaca.
Trombopenias.
Algunas conectivopatías
|
Complementary tests:
-
Skin tests (Prick tests):consist of exposing patients
to the suspected allergen through a micro-puncture made with a
lancet in the skin, usually in the forearm. They are safe and
specific, with an elevated negative predictive value (NPV).
The size of a positive reaction gives us some idea of the
patient’s degree of sensitivity to a specific allergen;
however, this varies greatly from patient to patient. In
addition, extracts can be made for testing for a large group
of allergens, which is very useful if we want to test for an
atypical allergen. The preparation of diagnostic food extracts
complicates the diagnosis. Purified allergens are better than
recombinants, which are obtained by recombining nucleic acids
in vitro. However, the latter are replicable and can be easily
standardised.
With fruits and vegetables, the prick by prick test is
preferable, bearing in mind that the peel is more allergenic than
the pulp, and that there are different levels of allergenicity
between varieties of the same species. If the reaction was
anaphylactic, it is better to avoid the tests and measure the
specific IgE instead.Intradermal reaction
tests are not used in food allergy testing because they
have not been shown to have diagnostic value and because they are
also dangerous, as they may trigger a systemic reaction
(Sicherer & Teuber, 2004).
Patch testing, useful for
assessing the cause of contact dermatitis, is also not commonly
used in the diagnosis of food allergy.
-
IgE quantification: There is a correlation between
the severity of clinical features and the presence of
specific IgE against a wide variety of foods.
These “in vitro” tests do not pose a risk of allergic
reaction, are not affected by the medication the patient may
be taking (antihistamines), and do not depend on the
characteristics of the skin. This is very useful
in paediatrics, especially in infants under 12 months of age,
where sensitisation is not clearly reflected on the skin using
the prick test. Specific IgE should not be confused with the
measurement of total IgE. Patients with any
type of allergic condition usually have very high levels of
IgE in comparison to the rest of the healthy
population. Although an elevated total IgE rate
indicates that the patient may be atopic, this rate does not
provide information about the patient's condition or which
allergens the patient is sensitive to. The usefulness of this
measure is limited, except for the diagnosis and follow-up of
some diseases, such as parasite infections, broncho-pulmonary
aspergillosis, hyperimmunoglobulin E syndrome, etc.)
Food-specific IgE is measured in levels of kU/L. Even if the
test is positive, the patient may not be allergic (average levels
may be found in food-tolerant patients). This is why clinical
records are essential. However, these tests have a high positive
predictive value in children
(Sampson & Ho, 1997.
-
Molecular diagnostics (component-resolved
diagnostics): Advances in recombinant protein research
have made it possible to identify different types of IgE that
bind to different epitopes or proteins in the same food.
Molecular diagnostics are a set of highly sensitive and
specific techniques that allow us to identify different types
of IgE against different molecules of a single food (while
distinguishing the potentially anaphylactic ones). These
techniques also allow us to establish a prognosis of allergic
symptoms. For instance, a patient may be hypersensitive to
hazelnut and have different types of IgE. If the patient has a
positive response to IgE Cor1, the patient will have very mild
oropharyngeal symptoms or will even be tolerant to hazelnut.
However, if the patient tests positive for IgE Cor 8, the
symptoms are likely to be more severe and the patient may
become anaphylactic because this protein is a lipid transfer
protein (LTP)
(De Knop et al., 2011)
(Hansen et al., 2009).
While molecular diagnostics techniques for plant foods are very
advanced, much remains to be done in the field of allergies to
animal foods. This is the most specific type of testing and is
highly sensitive, so the results obtained must be assessed by an
expert.
-
Elimination diets: of various types.
Elimination diets of the suspected food:
improvement of the symptoms is observed at 2 weeks if the
allergy is IgE mediated. In non-IgE mediated allergies,
improvement can be observed after several weeks of exclusion
(Lozinsky et al., 2015) .
This type of diet is practised in
paediatrics, especially when milk allergy is suspected, as
shown below. Empiric elimination diet: The
most potentially allergenic foods are removed from the diet
and then introduced one by one. This diet is mainly used in
chronic conditions (eosinophilic oesophagitis, chronic
idiopathic hives, etc.). This type of diet should only be
prescribed by a professional and should be monitored by a
nutritionist, especially in children, as the exclusion of
certain foods could affect their growth. Elemental
diet: food is replaced by extensively hydrolysed
amino acid formulas. It is used in very severe cases of food
allergy.
-
Food-controlled provocation tests are highly
diagnostic techniques (gold standard), but they involve risks.
They should not be performed in case of anaphylaxis or severe
systemic reaction, or in case the clinical record is highly
suggestive, repeated, recent, and consistent with a previous
allergological analysis.
-
Testing techniques that have not been shown to be
useful in the diagnosis of food allergy: The
determination of specific IgG, IgA, and
IgM is of no use. Cytotoxic testing
techniques (ALCAT) are not replicable and are not supported by
the scientific literature. Other testing techniques, such as
kinesiology, neutralisation,
and electrothermal pulse
have no value.
Food Allergy Treatment
Elimination diet: The current options available
for treating food allergy are based on avoiding the allergen and
waiting for the patient to become tolerant to the food over time.
In the natural course of food allergy, the period of clinical
sensitisation is followed by a period of asymptomatic
sensitisation, until total tolerance is achieved and specific IgE
antibodies disappear. Not all food allergy sufferers become
tolerant, in some cases, allergy tends to persist for years and
the longer symptomatic sensitisation is maintained, the less
likely it is to heal.
Substitution diet in food allergies: There are
some circumstances in which the use of special substitute
foodstuffs is necessary, as in the case of allergy to cow’s milk
proteins in infants. In this case, we will use a cow’s milk
protein hydrolysate until tolerance is achieved.
Periodic checks that tolerance has developed: In
young children, every 6-12 months. The periodicity varies
according to the clinical features of the allergy and the food
involved. This is necessary in order to establish whether it is
necessary to continue with the exclusion diet or, if the food is
tolerated, to add it to the diet safely.
Hyposensitisation: The food elimination diet has
many drawbacks in terms of compliance (many foods have hidden
allergens, especially the most processed), nutrition (by depriving
the child of certain foods), as well as the drawbacks arising from
family distress and the child rejecting the food itself once
tolerance has developed.
-
Specific oral immunotherapy (OIT)
treatments are based on introducing the food orally
at very small doses tolerated by the patient, while the doses
are progressively increased. Thus, tolerance can be achieved
while the amount of specific IgE decreases. These protocols
last approximately 3-6 months, but may last longer if the
patient is very allergic. These guidelines have been shown to
be very effective for the treatment of milk and egg
allergies.
-
Conventional immunotherapy. Immunotherapy
has been successfully tested in some types of allergy to plant
foods and has yielded good results in the treatment of
eosinophilic oesophagitis
(Armentia et al., 2018).
Prevention
Primary prevention (before the onset of allergy)
consists of the implementation of measures aimed at preventing
sensitisation to food allergens and the development of allergic
manifestations ensuing from such sensitisation. These measures are
particularly important in patients with a history of atopy.
Children with food allergy often develop atopic dermatitis and
other conditions that manifest over time (allergic conjunctivitis,
asthma, etc.). This is called the “allergic march.” For this
reason, the professional in charge of these high-risk children
should propose dietary standards aimed at avoiding sporadic
contact with minimum doses of potentially sensitising foods. In
addition, this professional should be the first person in the
lookout in the event of an allergic reaction to food.
Secondary prevention: Elimination diet is not the
only element to take into account when monitoring an allergic
patient, but also the occurrence of new sensitivities on contact
with new foods. One case in point is that of children allergic to
cow’s milk: exclusive breastfeeding up to 6 months (or,
alternatively, hydrolysed milk) should be promoted, after which
the foods should be introduced progressively and separately (one
or two weeks must pass between each food), with repeated daily
portions. Subsequently, it is necessary to maintain contact with
all the foods that the child eats at least two days a week.
BRIEF RECOMMENDATION IN RESPONSE TO THE ORIGINAL
QUESTION
The optimal follow-up of a child with food allergy requires the
collaboration of the paediatrician and the allergist, and in order
to find the correct aetiology, valid diagnostic techniques must be
used. Oral food immunotherapy is to be performed in Allergy
Units.
Acknowledgment
This publication has been possible to the cooperation program Interreg VA España-Portugal POCTEP - RISCAR 2014-2020.
http://www.poctep.eu
References
-
Worm, 2014Worm, M. Immunology., European Academy of allergy and Clinical. Zurich: Global Atlas of Allergy. Reacciones a aditivos de alimentos y medicamentos.
-
Martín Mateos, 2011Martín Mateos, M. A. ergon. Tratado de alergología pediátrica.
-
Pyrhönen, Näyhä, Kaila, Hiltunen, & Läärä, 2009Pyrhönen, Kaisa, Näyhä, Simo, Kaila, Minna, Hiltunen, Liisa, & Läärä, Esa. (2009, 06). Occurrence of parent-reported food hypersensitivities and food allergies among children aged 1-4 yr. Pediatric Allergy and Immunology,
20
(4), 328, 10.1111/j.1399-3038.2008.00792.x, 19538354.
-
Leung, Yung, Wong, Lam, & Wong, 2009Leung, Ting Fan, Yung, Edmund, Wong, Yun Sze, Lam, Christopher W. K., & Wong, Gary W. K. (2009, 06). Parent-reported adverse food reactions in hong kong chinese pre-schoolers: Epidemiology, clinical spectrum and risk factors. Pediatric Allergy and Immunology,
20
(4), 339, 10.1111/j.1399-3038.2008.00801.x, 18808390.
-
Venter et al., 2006Venter, Carina, Pereira, Brett, Grundy, Jane, Clayton, C. Bernie, Roberts, Graham, Higgins, Bernie, & Dean, Taraneh. (2006, 05). Incidence of parentally reported and clinically diagnosed food hypersensitivity in the first year of life. Journal of Allergy and Clinical Immunology,
117
(5), 1118, 10.1016/j.jaci.2005.12.1352, 16675341.
-
Nwaru et al., 2014Nwaru, B. I., Hickstein, L., Panesar, S. S., Roberts, G., Muraro, A., & Sheikh, A. (2014, 08). Prevalence of common food allergies in europe: A systematic review and meta-analysis. Allergy,
69
(8), 992, 10.1111/all.12423.
-
SEAIC, 2015SEAIC, . (2015). Informe alergológica 2015. Sociedad española de alergología e inmunología clínica.
-
Sicherer & Teuber, 2004Sicherer, Scott H., & Teuber, Suzanne. (2004, 11). Current approach to the diagnosis and management of adverse reactions to foods. Journal of Allergy and Clinical Immunology,
114
(5), 1146, 10.1016/j.jaci.2004.07.034.
-
Sampson & Ho, 1997Sampson, H A, & Ho, D G. (1997, 10). Relationship between food-specific ige concentrations and the risk of positive food challenges in children and adolescents. The Journal of allergy and clinical immunology,
100
(4), 444, 10.1016/s0091-6749(97)70133-7, 9338535.
-
De Knop et al., 2011De Knop, K. J., Verweij, M. M., Grimmelikhuijsen, M., Philipse, E., Hagendorens, M. M., Bridts, C. H., De Clerck, L. S., Stevens, W. J., & Ebo, D. G. (2011, 02). Age-related sensitization profiles for hazelnut (corylus avellana) in a birch-endemic region. Pediatric Allergy and Immunology,
22
(1pt2), 10.1111/j.1399-3038.2011.01112.x, 21342279.
-
Hansen et al., 2009Hansen, Kirsten Skamstrup, Ballmer-Weber, Barbara K., Sastre, Joaquin, Lidholm, Jonas, Andersson, Kerstin, Oberhofer, Hubert, Lluch-Bernal, Magdalena, Östling, Jonas, Mattsson, Lars, Schocker, Frauke, Vieths, Stefan, & Poulsen, Lars K. (2009, 05). Component-resolved in vitro diagnosis of hazelnut allergy in europe. Journal of Allergy and Clinical Immunology,
123
(5), 1134, 10.1016/j.jaci.2009.02.005, 19344939.
-
Lozinsky et al., 2015Lozinsky, Adriana Chebar, Meyer, Rosan, De Koker, Claire, Dziubak, Robert, Godwin, Heather, Reeve, Kate, Dominguez Ortega, Gloria, & Shah, Neil. (2015, 08). Time to symptom improvement using elimination diets in non-ige-mediated gastrointestinal food allergies. Pediatric Allergy and Immunology,
26
(5), 403, 10.1111/pai.12404, 25963794.
-
Armentia et al., 2018Armentia, A., Martín-Armentia, S., Martín-Armentia, B., Santos-Fernández, J., Álvarez, R., Madrigal, B., Fernández-González, D., Gayoso, S., & Gayoso, M.J. (2018, 03). Is eosinophilic esophagitis an equivalent of pollen allergic asthma? Analysis of biopsies and therapy guided by component resolved diagnosis. Allergologia et Immunopathologia,
46
(2), 181, 10.1016/j.aller.2017.11.001, 29338961.

 License Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International
License Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International