
Luis Torres Pérez, Mónica Rodríguez Bouza, Ana María Leal Valle, Jesús Bujalance Hoyos and Cipriano Viñas Vera
Emergency Management: Introduction
Abstract: AbstractThe present article summarises the immediate
management of vomiting in paediatric patients from the Paediatric
Assessment Triangle approach, including the primary and secondary
assessments of signs and symptoms for handling the situation properly.
The relevant articles on the subject have also been updated.
Keywords: Uncertainty; Patient Preference; Pediatric Nursing
IMMEDIATE MANAGEMENT
Managing uncertainty in paediatrics is a challenge for any
clinician. Being able to discern between low complexity cases, with
more or less complex features, and the cases that require
supervision by a specialist (or which represent a threat) is a very
frequent problem in primary care.
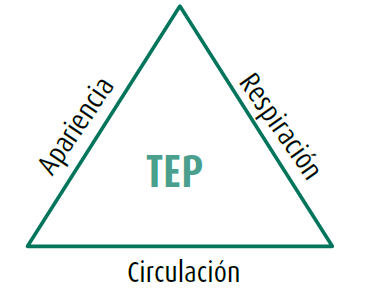
The Paediatric Assessment Triangle (PAT) attempts to systematise
the concept of “great diagnostician” attributed to the clinical
expert. This is a useful, quick, and simple assessment method that
identifies the type and severity of the problem and prioritises the
initial treatment
(Figure 1. The Paediatric Assessment Triangle PAT)
( Figure 1. The Paediatric Assessment Triangle PAT Translation)
The PAT formally categorises the general impression of the
patient’s condition in line with the fact that emergency management
requires a shift in approach in order to focus on what the patient
needs rather than on what the patient has.
Figure 1. The Paediatric Assessment Triangle (PAT)
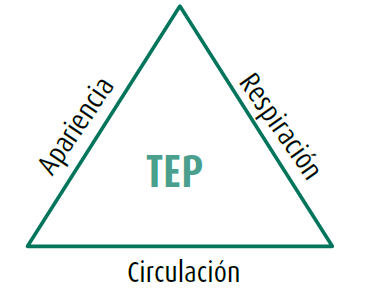
Source: Horeczko, Enriquez, McGrath, Gausche-Hill, & Lewis, 2013
Table 1. Figure 1. The Paediatric Assessment Triangle PAT Translation
| Spanish |
English |
| TEP |
PAT |
| Apariencia |
Appearance |
| Respiración |
Breathing |
| Circulación |
Circulation |
The TAP is based on audio-visual examination, without using hands
or any other element. The assessment of the appearance, the analysis
of the work of breathing, and the appearance of the skin as
indicators of circulatory status make up the three sides of the
triangle.
The approach of these bulletins is focused on patients with a
stable clinical situation in which primary and secondary assessments
will allow us to follow an effective and purpose-oriented
therapeutic approach in the majority of cases
(Horeczko, Enriquez, McGrath, Gausche-Hill, & Lewis, 2013)
DEVELOPMENT
Appearance assesses tone (if the child moves spontaneously,
resists examination, is seated or standing, etc.), interactiveness
(if the child is alert and connects), consolability, look/gaze (if
the child makes contact, if there is visual tracking), and
speech/crying (loud crying, inappropriate words, etc.).
The analysis of the work of breathing consists of observing the
position adopted by the child (on a tripod, not tolerating
decubitus, etc.), any pulling, nasal flaring, or head nodding, as
well as any abnormal respiratory noises (whimpering, hissing, nasal
voice) that can be heard without the need for auscultation with a
stethoscope.
Circulatory status is assessed based on the appearance of the
skin: Is there pallor? Is it cyanotic? Does it present with cutis
marmorata (a marble-like complexion)?
These factors provide a benchmark for cardiac output and organ
perfusion
(Carles Luaces Cubells, Montse Delgado Maireles, Yolanda Fernández Santervás, 2015)
(Cázares-Ramírez & Acosta-Bastidas, 2014)
CLINICAL ORIENTATION: SUMMARY
(Table 2. Orientation according to the PAT)
Table 2. Orientation according to the PAT
| Appearance |
Work of breathing |
Circulation |
Clinical orientation |
| N |
N |
N |
Stable |
| A |
N |
N |
CNS dysfunction |
| N |
A |
N |
Shortness of breath |
| A |
A |
N |
Respiratory failure |
| N |
N |
A |
Compensated shock |
| A |
N |
A |
Decompensated shock |
| A |
A |
A |
Cardiopulmonary failure |
PRIMARY AND SECONDARY ASSESSMENTS
Primary paediatric assessment uses the Airway, Breathing,
Circulation, Disability, Exposure (ABCDE) approach for
assessment and management.
Primary paediatric assessment is a practical assessment of
respiratory, cardiac, and neurological function, including
assessment of vital signs and determination of oxygen saturation
(Cázares-Ramírez & Acosta-Bastidas, 2014)
This part of the primary evaluation includes the following
(Table 3. Management summary):
-
ABCDE assessment:
-
Intervention/action: initiation of treatments
-
First letter in each of the sections.
-
Identification of threatening problems:
categorisation
In this method, thorough examination (use of hands) is added to
observation.
S: signs and symptoms.
A: allergies.
M: medications.
P: pertinent past medical history.
L: last oral intake.
E: events leading to present illness/injury. This
must include the mechanism of the injury, the time it occurred,
and what happened until the child became cared for.
This gives way to a complete examination and assessment of the
patient’s situation and whether there is a need for transfer to or
management at another level of care.
Table 3. Management summary
| The Paediatric Assessment Triangle (PAT) |
|
|
| Primary assessment: ABCDE |
-
A: patent airway and cervical stabilisation
-
B: ventilation and oxygenation
-
C: circulation and haemorrhage control
-
D: neurological dysfunction
-
E: exposure
|
| Secondary assessment |
|
|
| Categorisation and transport |
|
|
Acknowledgment
This publication has been possible to the cooperation program Interreg VA España-Portugal POCTEP - RISCAR 2014-2020.
http://www.poctep.eu
RINSAD
The Journal of Childhood and Health
(Revista Infancia y Salud - RINSAD),
ISSN: 2695-2785, arises from the collaboration between the
administrations of Portugal, Galicia, Castilla y León, Extremadura,
and Andalusia, within the
Interreg
Spain-Portugal RISCAR
project, and aims to
disseminate scientific articles on children’s health, providing
researchers and professionals with a scientific base from which to
learn about the latest advances in their respective fields.
The two main target audiences of RINSAD are:
-
Researchers in the field of childhood and health.
-
Professionals in the sector.
Total cost of the project (indicative): 2,418,345.92 €
Total ERDF approved: 1,813,759.48 €
RINSAD is the result of the
Interreg
Spain - Portugal RISCAR
project in collaboration
with the
University
of Cádiz
and the
Nursing
and Physiotherapy Department of the University of
Cádiz
, Cádiz, Spain.
The works published in this journal are licensed under a
Creative
Commons Attribution-NonCommercial-ShareAlike 4.0
International
license.
References
-
Carles , Luaces Cubells, Montse , Delgado Maireles, & Yolanda , Fernández Santervás. (2015). Urgencias pediátricas de atención primaria en coordinación con el Hospital Sant Joan de Déu. Hospital Sant Joan de Déu,
https://www.sjdhospitalbarcelona.org/sites/default/files/u1/Para_profesionales/Programas_otros_centros/01_2015_06_09_urgencias_pediatricas_ap_hsjd_cast.pdf
.
-
E. , Cázares-Ramírez, & M.A. , Acosta-Bastidas. (2014). Valoración pediátrica inicial en Urgencias. Acta Pediátrica Mexicana, pp. 82-87,
35
(1),
http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0186-23912014000100013
.
-
The Pediatric Assessment Triangle: Accuracy of Its Application by Nurses in the Triage of Children. (2013, 03). pp. 182-189,
39
(2), doi:10.1016/j.jen.2011.12.020, HoreczkoTimothyEnriquezBriannaMcGrathNancy E.Gausche-HillMarianneLewisRoger J., Journal of Emergency Nursing.
-
Atención inicial al paciente traumatizado grave, 2015P., Storch de Gracia Calvo. (2015). APap - Formación Activa en Pediatría de Atención Primaria (Vol. 39). Madrid: APap. 2, pp. 182-189, Atención inicial al paciente traumatizado grave.

 License Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International
License Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International